August 21, 2021 |
|
|
On Tuesday, August 3rd, Nancy drove me to Seattle for a day of appointments at Seattle Cancer Care Alliance (SCCA) and Swedish Orthopedic Institute. Unfortunately, we hit heavy traffic as we approached downtown Seattle, missing the too-late Google Maps suggestions for taking alternate routes. Having left plenty of time, we still arrived 15 minutes early. My day usually begins at SCCA with a blood draw in the first-floor lab. Whenever I check in, the receptionist asks me if I will need an IV. On this day, I realized I would need an IV because my doctor had scheduled me for a Zometa infusion later in the day. She is treating me for osteopenia (bone density loss) caused by the hormone deprivation therapy I have been on for two and a half years. A young man called my name and brought me into the lab. I took a seat in the specially built recliner chair with an armrest in front for drawing blood and putting in IVs. As he attempted to insert the first IV, I told him that this was hallowed ground for me. He curiously asked me why. I told him about my head injury thirty-seven years before on the curb across the street from the building. After failing on his first IV attempt, he found a new vein and began his second attempt. Maybe I distracted him too much from his work because he was unable to put in the second IV successfully. He told me that they only allowed each nurse two attempts and that he would have to go and call another nurse. The next nurse came, taking the other arm, and made two attempts. On her second try, she had found a vein in my left forearm and gave a valiant effort to insert the IV. After what seemed like over a minute, she said she had likely hit a valve and withdrew the needle. Since it was her second try, she left to get a third nurse. After four attempts, with the last one quite painful, I began feeling nauseous, breaking out in a cold sweat, and feeling like I was going to faint. When the nurse came back with the third-tier nurse, he said to me, “You look very clammy!” I responded, “Am I a nice shade of grey?” They called for other nurses to come, putting the recliner back, so my head was below my body. They put an ice bag behind my neck and a cold, wet washcloth on my forehead. While I was distracted by the other nurses and their care, the third-tier nurse promptly inserted the IV in the back of my left arm. |
|
 |
|
|
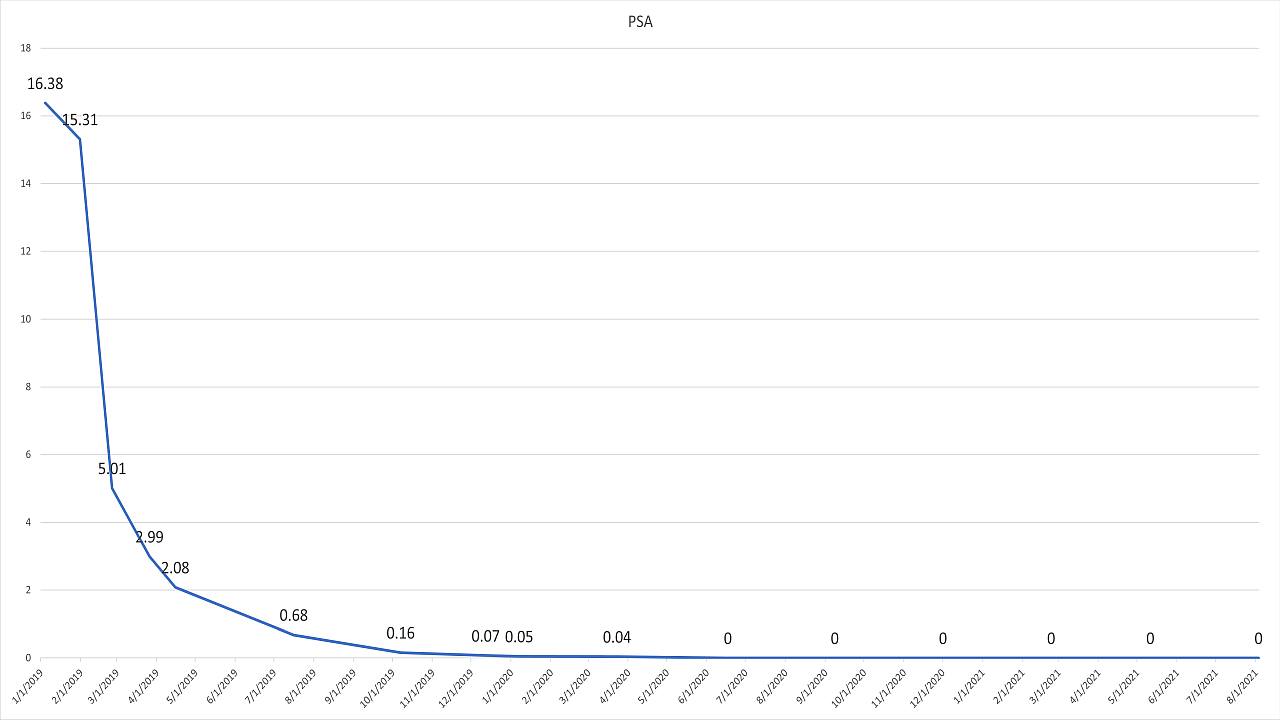
After enough time to recover, they escorted me out to the waiting room. Nancy and I went to the third floor to wait for my appointment with my nurse practitioner. When we met with her, we learned that my PSA was again undetectable! Nancy and I were thrilled. Later in the afternoon, I had the Zometa infusion, an uneventful procedure that took about fifteen minutes. On our way home, we stopped at Seattle Orthopedic Institute for my appointment with my orthopedic surgeon, who had replaced my right hip in January of 2020. After taking x-rays, he said that the hip replacement looked great. So, what started as a trying day stuck in heavy Seattle traffic and enduring five IV attempts ended with a couple of welcome reports! The following day, I awoke with severe spasms in my left forearm at the site of the fourth IV attempt. Each spasm would last two to three seconds, abate for a second or two, and then spasm again. The eight-out-of-ten pain had prompted me to jump out of bed with Nancy coming quickly to my side. After ten to twelve spasms, the pain subsided, only to return every five minutes. The painful spasms continued for two hours, during which Nancy called my nurse at Seattle Cancer Care Alliance. As the two hours progressed, I began to have chest pain which radiated up my neck and down into my left arm. The nurse instructed Nancy to call my cardiologist, who recommended that we go to the emergency room. Nancy drove me to St. Michael’s Medical Center in Silverdale, a newly built, state-of-the-art hospital in Silverdale. Upon arrival, the intake nurse quickly put me in a triage room. A nurse came in, drew blood, and then ran an EKG—which came back without any abnormalities. They then transferred me into one of the forty-eight ER rooms. About twenty minutes later, a technician arrived who announced that he was taking me for a CT scan with contrast. Within ten minutes after arriving back in my room, the doctor came into the room and informed Nancy and me that I had multiple small pulmonary embolisms (blood clots) across both lungs. He would be admitting me to the hospital after starting a Heparin drip, a powerful blood thinner to prevent the clots from growing. Nancy and I were shocked. After a lengthy interview with the doctor, he determined that the cause of the embolisms was likely my having advanced cancer, which predisposes cancer patients to blood clots. |
|
 |
|
|
The doctor admitted me to the hospital, where I received excellent care from the doctors, nurses, CNAs, and phlebotomists. The hospitalist kept me on the Heparin drip for forty-eight hours and then discharged me from the hospital on a new blood thinner—which I will be taking for the rest of my life. After arriving home, Nancy told me how relieved she was that I had survived having multiple blood clots in both lungs. I was gracefully ignorant of the dangers of having blood clots in one’s lungs. As the gravity of what had happened sunk in, I found myself grateful for two nurses and their failed attempts at putting an IV in my arm. I am so thankful for the nurse who dug around in my left forearm, thereby traumatizing the vein, which resulted in my waking with severe spasms the following day. I am grateful for the ensuing chest pain, which ended up amounting to nothing, but was enough to motivate us to go to the emergency room. If the doctor had not found the blood clots, they would have likely grown, causing damage to my lungs and heart, with the potential to bring about my death. On this last Sunday, late in the evening, I returned to the emergency room with an increased tightness and pressure across my chest and with chest pain shooting up my neck and down my left arm. They again admitted me to the hospital for two days of tests. After taking a second CT scan with contrast, they discovered that the pulmonary embolisms were gone, dissolved by my body. All the tests showed that the condition of my heart is unchanged. They determined that the inflammation from the blood clots, exacerbated by two days of heavy smoke in our area, coupled with my exhaustion, had brought on the chest pain. |
|
 |
|
|
After the nurse had brought me into the room in the emergency department at St. Michael’s this past Sunday, I commented to Nancy, “The LORD is my shepherd, I shall not want. He makes me lie down in white hospital beds.” She looked over and said, “Grant, you are lying on green sheets!” I turned my head and looked at the sheet on which I was lying and saw a dark green sheet. “The LORD is my shepherd. I shall not want. He makes me lie down in green hospital beds. He leads me beside stills waters. He restores my soul.” When Jesus is our shepherd, He begins with providing us rest and sustenance, followed by times of refreshment, solitude, and peace. Then, before any work, without obligation, because He is the Good Shepherd who loves us more than we can know, He restores our souls, healing our broken and agitated minds, wills, and emotions. He makes me lie down in green hospital beds! |
|
© 2022 by Grant Christensen. "Freely you have received, freely give." (Matthew 10:8b NIV) You are free to share--copy and redistribute in any medium or format--as long as you don't change the content and don't use commercially without permission of the author or author's family. |
|